Nursing Vacancies Decline in the Bay State, But The Problem Persists
The Massachusetts Hospital Association (MHA) recently reviewed the financial records of hospitals across the Common-wealth, and found that from October 2003 to March 2004, 53{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5} were operating in the red.
In late September, the MHA reported that Massachusetts hospitals were suffering due to rapid rises in costs, ranging from medical supply and pharmaceutical prices, to high labor expenses driven by a competitive market with significant shortages. Further, the MHA reported the problem is exacerbated by reimbursements and payments that aren’t keeping pace with those increases.
Western Mass. hospitals are feeling the squeeze as much as any facilities in the state, if not more in some respects. And while some providers have managed to stay in the black, health care professionals in the area say that the financial pressures put on hospitals have only worsened in recent years, and moreover, those pressures create new challenges each day.
Cause and Effect
Bob Blondin, vice president of finance at Noble Hospital in Westfield, said operating a hospital is much like operating a household; any increase in standard expenses is going to force a tightening of the purse strings. The two recurring expenses that have hit facilities the hardest in recent years, Blondin said, are those of pharmaceuticals and staffing.
The pharmaceutical advertisements that can be seen in every newspaper and on every television channel, touting the newest drugs, are excellent indicators of the state of the pharmaceutical industry, added Blondin.
“Pharmaceutical costs are up 10{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5} over last fiscal year,” he said. “That really hurts us. There are new drugs coming out constantly, and they are more and more expensive. The advertising budgets alone of many pharmaceutical companies are huge – and the ads obviously work. We’re talking about an unregulated industry here, and the health care industry has little leverage.”
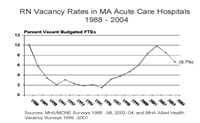
And as pharmaceutical and medical supply rates soar, the health care labor shortage persists. Blondin said the lack of nurses and other professionals, such as technicians, is constantly at the forefront of Noble’s financial picture, because the shortages factor into so many aspects of the industry.
First, the shortages have created the equivalent of a buyer’s market for job seekers in the health care field. Blondin said hospitals now have to work doubly hard to market their organizations, recruit new staff, and to retain employees as well.
“We try to recruit and retain the right mix of doctors, nurses, and other staff, but everyone else in the area is doing the same thing,” he said. “It’s very hard for small hospitals like us to keep up.”
In turn, while hospitals work to recruit potential employees in order to fill the staffing gap, many hospitals are being forced to employ large numbers of contract laborers, or temporary employees, in the meantime to maintain adequate staff numbers. Those contract employees, Blondin said, usually demand higher salaries than regular full-time employees.
“Outside contract labor agencies cost double of what we normally pay,” he explained. “That really hurts us.”
Blondin said Noble Hospital just completed the third fiscal year at which the facility has operated at a loss, and one of the largest costs incurred last year was a whopping $700,000 in contract labor expenses. Labor costs in general account for approximately 60{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5} of total hospital expenses statewide, according to the MHA.
In addition to recurring costs, reimbursement rates at both state and federal levels are lagging. Blondin said Massachusetts’ Medicaid system pays about 65 cents on the dollar in terms of the cost of patient services, and he said studies suggest that gap will only get wider in coming years. Further, the recent unenrollment by the state of thousands of MassHealth customers caused the state’s free care pool to deepen significantly.
“Those customers became uninsured,” Blondin said. “Patients without insurance are entitled to receive free care based on income, family size, and some other variables, so essentially the health care industry had to eat those costs.”
“The free care pool is overtaxed,” added Craig Melin, president and CEO of Cooley-Dickinson Hospital. “And under-insurance is also a problem. Only a certain percentage of patients with private insurance that pay at or above the cost of a patient’s care can offset the shortfalls in revenue caused by Medicare and Medicaid; at Cooley-Dickinson, we are about middle of the road in that respect, but in Holyoke and Springfield, where there are higher numbers of uninsured patients, the shortfalls are even worse.”
With costs up and reimbursements down, Western Mass. hospitals are more or less on par with hospitals in the rest of the state in terms of operating margins; some, like Cooley-Dickinson, have turned a profit, but even those facilities performing well in the area compare poorly against leading hospitals in other states, according to the MHA. The median operating margin in Massachusetts is roughly 1.8{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5}; well below national benchmarks, and also well below the MHA’s recommended 3{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5} minimum margin.
In order to reduce costs and help close the gap created by low reimbursement rates and high costs of service, many hospitals are looking more toward employee retention in order to curb contract labor costs and the expenses associated with recruitment. Melin said his organization actually increased the number of full-time employees on staff, replacing 27 temporary staffers with 60 full-time equivalent workers.
“It sounds like it should cost more, but it reduced our labor costs,” he said, adding that the move also created a positive ripple in the overall culture at the hospital. “Because nurses and other employees knew the hospital and became part of the team, they were more satisfied with their jobs. Then patient satisfaction went up, and volume went up. Those increase numbers brought in revenue that helped balance our budget.”
Vince McCorkle, president and CEO of Mercy Medical Center, agreed that attention to a hospital’s overall philosophy may be a less tangible financial solution than cutting services or workforces, but he too has seen the practice create positive changes.
“We constantly revisit our mission statement,” he said. “We make decisions based first on service to patients.”
McCorkle said a committee dubbed ‘Mission Critical’ has also been formed at Mercy to address not only financial concerns, but challenges facing health care at all levels.
“When in adverse situations, it takes diligent, day-to-day management of operations to drive performance,” he said. “The members of the group take it very seriously … it’s a matter of management, but it is also a matter of integrity.”
At Any Rate
Several Western Mass. hospitals also took a hit last year that was unique to the area, and created an even greater strain on operating budgets. Medicare, of which approximately 45{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5} of local residents carry, reclassified two Massachusetts hospitals last year, located on Nantucket and Martha’s Vineyard, which removed them from ‘rural’ classification and renamed them ‘critical access facilities.’ The reclassification, according to Melin, lowered the wage index many area hospitals were functioning within, and in turn lowered Medicare reimbursements to those hospitals.
“Normally, when Medicare shifts someone out of a classification, there is an extended transition time, and time to adjust,” Melin said. “This time though, they yanked those two hospitals immediately. The rural rate dropped because those two hospitals dropped out …all of the area hospitals had been bolstered by that rate, and we lost that security all at once.”
All Western Mass. hospitals that had been classified in the same wage index as the two island hospitals – including Noble, Cooley-Dickinson, and Mercy Medical Center – saw losses due to that reclassification. McCorkle said Mercy saw a negative impact totaling $1.4 million.
Checks and Balances
Keeping a close watch on costs is one hurdle hospitals must clear, but financial forecasts are made more cloudy by the need to provide a service unlike any other in the American landscape: safe and effective medical care, despite any and all adverse conditions.
“We have to keep giving raises, and other costs keep going up,” said McCorkle, adding that despite both constant and unexpected financial hardships like the rural rate reclassification, all hospitals must continuously update medical equipment and technology, maintain a strong staff base, and above all, continue to work to keep patients healthy. “We have to stay competitive, or we can’t function. In order to do that, hospitals essentially end up consuming all of their past harvests. At the same time, we need to take the values of practice very, very seriously.”