Health Graduates Enter the Field at an Anxious Moment
Trial by Fire
By Joseph Bednar
Tallon Tomasi used to punch the same clock everyone else does when starting her shift as an LPN at the Leavitt Family Jewish Home in Longmeadow.
Not anymore. Because she works in a COVID-positive unit at the skilled-nursing facility, she enters by a different way than those in the negative units.
“Now, when we come in, we do this check-in system where we wash our hands, get our temperatures taken, we’re asked about symptoms related to COVID, about recent travels, recent exposure to people who have traveled. Then we get our gear, we wash our hands, and go to work.”
As a nursing student at Holyoke Community College, Tomasi is just beginning her healthcare career, and doing so right on the front lines of a global pandemic the likes of which haven’t been seen in more than a century.
Some aspects of it are tough to bear.
“The thing that’s very hard is not having family members being able to come in and see their loved ones as we are going through this difficult time,” she told HCN. “Some of our patients have dementia, and not being able to see their families, it is challenging.”
That said, “I think our facility has done a good job,” she went on. “We do phone calls with family, and we do FaceTime, so I think that helps a little bit. But not being able to physically touch loved ones is hard for some of the patients and their family members.”
Tomasi paused to consider what else has been challenging about working in healthcare during the time of COVID-19.
“Everyone is so fearful of not knowing what’s going to happen,” she finally said. “That’s a big problem. We are not fully aware of how this thing will go, how to treat it, so the new big problem is fear — fear of the unknown. We don’t know everything about it, there’s anxiety around it, and I sometimes get scared because I know that I have the ability to spread it. But you know what has to be done — you have to help.”
With graduation — such as it is this year — just around the corner, many more nurses and other healthcare professionals are getting ready to transition from college into full-time work, but they’re facing an uncertain job market when so much of the sector’s energy is tied up in simply containing the pandemic.
“I checked in with some of our soon-to-be-graduates, and as far as the job market goes, I would say it’s pretty much up in the air and confusing,” said Kathleen Scoble, dean of the School of Nursing at Elms College.
On one hand, she noted, Hartford Hospital and St. Francis Hospital just down I-91 have responded “pretty expeditiously” to graduating seniors, several of whom landed positions right away. On the other hand, Baystate Medical Center has informed applicants that its new-graduate nursing program, traditionally a very popular landing spot for Elms grads, has been postponed.
“We have mechanisms to do more triage and problem solving with patients before they come to a place where they’re exposing themselves to others.”

But the need is great, she added, and Elms President Harry Dumay agreed, adding, “I’m proud of being part of this sector and proud of not only our institution, but all students and graduates on the front lines during these difficult times.”
Even if, as we’ll see, it can be a little challenging getting to those front lines.
Field Work
For Springfield Technical Community College, which boasts the largest health-simulation center in the Northeast, students not having access to campus means not being able to use those tools in their training, President John Cook said.
“That does hinder the potential of our students to finish, graduate, and work in these fields, which, if they weren’t in demand before, are certainly in demand now.”
That’s a major factor in nursing right now, Scoble said.
“If you ask students what our major responsibility is, it’s preparing them for licensure; it’s our primary responsibility as a program, to make sure they meet all their graduation requirements. And that has been a keen challenge the last semester; all of our clinical learning experiences were canceled — understandably.”
Carol Leary, president of Bay Path College, also noted that nursing students have had their clinicals put off — and there’s only so much that can be accomplished online.
“For me, that is a concern because many of them need to sit for their licensing exams before they can begin to work,” she said. “The accrediting bodies are trying to work with all the programs across the country to figure out how students can sit for exams.”
Scoble noted that only one testing site is open in the entire state where nursing students can take their licensing exam, known as the NCLEX, and that site is following CDC requirements for social distancing. “So you can imagine, with thousands of nursing graduates in the state, how long it will take for them to test the class of 2020. But they’re trying to open as many sites as they can.”
In Gov. Charlie Baker’s guidance when shuttering the Massachusetts economy in March, language was included allowing new nurses to practice without a license, if supervised by a professional nurse of equal or higher education.
“It’s really up to the employers how they would receive a new graduate who is not licensed, how they would recruit and receive them,” Scoble said. “We would provide any supporting documentation they would require.
In the past, she explained, a typical student would agree to a position in early spring, then take the exam in June and start work around July.
“All that is unknown right now. Students would say the only thing they can control is finishing the program and preparing for NCLEX. We’re stressing to our soon-to-be-graduates to prepare for the NCLEX — and continue to prepare — until they have the opportunity to sit for the exam.”
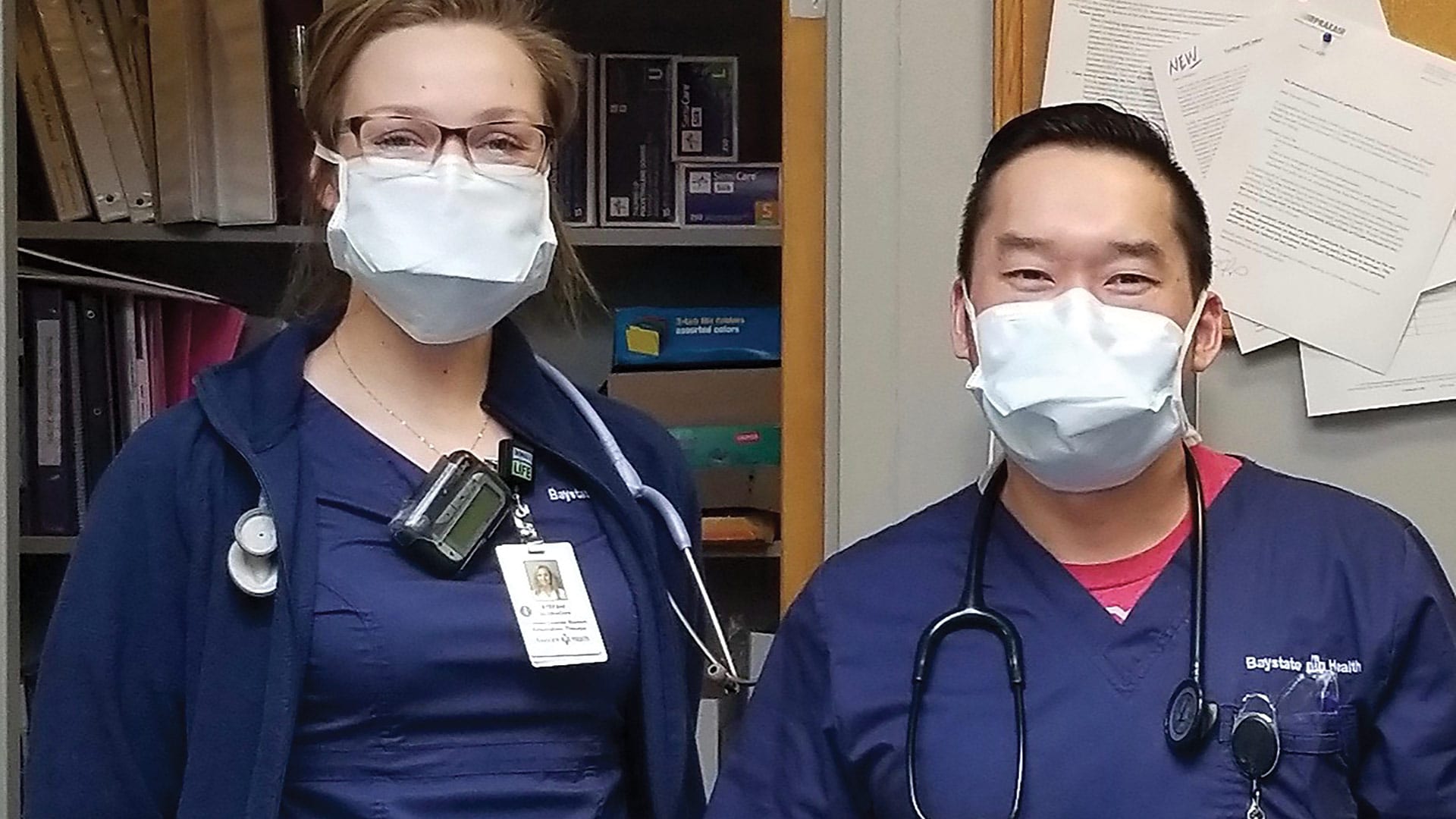
In a similar situation, three respiratory-care students from STCC recently began working at Baystate Medical Center after applying for and receiving limited permit licenses, said Esther Perrelli Brookes, director and department chair of the Respiratory Care program. Eight other students have applied for limited permit licenses so they can work in the field.
“Students chose to study respiratory care because they want to help people. They want to make a difference,” Perrelli Brookes said. “I’m extremely proud of my students who are stepping up during this unprecedented health crisis. I’ve had many students reach out to say they want to find out what they can do now. I’ve been helping them get their limited permit licenses.”
“I was one of the first in my class to do it,” student Max La said. “It’s a good learning experience because other respiratory therapists are there and you can learn from them.”
The limited permit license means he can perform certain tasks, but not everything a fully licensed respiratory care therapist would do. “We can’t touch the ventilators,” he said, referring to the devices that some seriously ill COVID-19 patients use in hospitals.
At Baystate, La does not work with COVID-19 patients, but must wear a gown, mask, and other personal protective equipment (PPE), and he said Baystate takes precautions to protect him and others from contracting the coronavirus. “There’s always concern, but Baystate has a good policy. Everyone has masks, and they do temperature checks when everyone is walking in.”
STCC’s respiratory care program trains students skills in treatment, management, diagnosis and care of patients with breathing problems associated with diseases such as COVID-19.
According to the U.S. Bureau of Labor Statistics, respiratory therapists will continue to be in high demand at hospitals and medical facilities, with job growth of 21% projected between 2018 and 2028 — and that was before COVID-19 wrought what is essentially a respiratory crisis around the globe.
Seeds of Change
Demand should remain high in many health fields, said Brooke Hallowell, dean of the School of Health Sciences at Springfield College, though it may be uneven in the short term. Take physical and occupational therapists — in emergency-care settings, they’re playing an important role in patient care. But those who work with post-surgical patients for, say, joint replacement may find work more intermittent as many elective procedures are being postponed.
One area of growth is in the realm of telehealth, she added. “All of our health professionals are going through a rapid transition in terms of telehealth access, and Medicare and insurance companies are adjusting their policies related to telehealth, and reimbursement for telehealth visits is being revamped.”
These efforts are intended to reduce the spread of COVID-19, but the lessons being learned may be long-term, Hallowell noted.
“Instead of waiting in a room full of sick people to be seen at the doctor’s office, we have mechanisms to do more triage and problem solving with patients before they come to a place where they’re exposing themselves to others. I think this is here to stay … how we carry out our practices will be changing in big ways.”
Interest in some health programs may shift as well, she added. For example, cardiopulmonary rehabilitation, a specialty within physical therapy, is getting more attention for the vital role it plays in COVID-19 treatment. And Springfield College is probably launching its new undergraduate program in public health this fall at the right time, too.
“We expect that will be a popular major, as people become more aware of what public health and epidemiology are,” Hallowell said. “That’s good timing for us.”
Christina Royal, president of Holyoke Community College, told HCN that a great deal of first responders, nurses, and other healthcare workers have taken classes at community colleges like HCC at some point.
“When I think about our role in ensuring that we have the workforce talent we need in healthcare, which is the primary sector in Western Mass., I think it’s important that we continue to think about the kind of training we’re doing and how to continue to support this community.”
Scoble doesn’t foresee a time when nursing is not an in-demand profession.
“I’m not sure what we’re going to experience over the next few months,” she said. “A lot has to do with how we come back as a country, as a state, and as a community, but I have no doubt that every single one of my graduates will land a position at some point. If this was a normal period of time, a normal spring, many of the graduates would be on the fringe of accepting a position. They would have had interviews and been called back. Right now, a lot of that is at a standstill.”
When they do land jobs, Scoble added, “they’ll have the knowledge and skills and competencies, but lack a great deal of experience. So my number-one concern is, will they enter a work environment where they have the kinds of orientation and support they need? It’s definitely a concern.”
Stefani Glukhova, one of STCC’s respiratory-care students who started working at Baystate in March, may put some of those concerns to bed.
“All the staff here are very kind and generous and are always willing to help you,” she said. “As it gets busier at the hospital with fighting COVID-19, the registered respiratory therapists work around the clock to help fight the virus. My fellow classmates and I do our very best to be available and help out with treatments, floor therapies such as chest physical therapy, and much more.
“This is an amazing learning experience that I would recommend,” she concluded — even if it comes during a pandemic that no one would ever recommend.


