As Delta Variant Lingers, Hospitals Gird for an Uncertain Fall
Crowd Control
By Joseph Bednar
More than 18 months into the pandemic, not much about COVID-19 surprises doctors anymore, but this coming fall — with schools and colleges welcoming students back, concerts and large gatherings ramping up, and the Delta variant still raging — still poses some uncertainty.
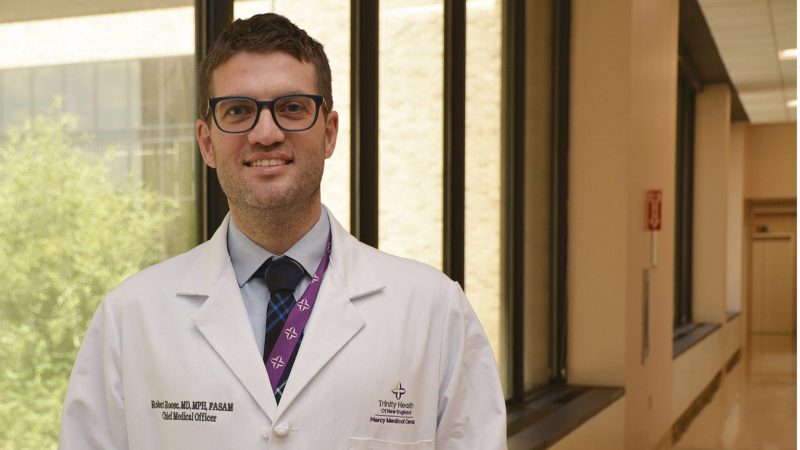
And Dr. Robert Roose says the medical community is ready.
“We’ve been in a constant state of readiness since January of 2020, and we’ve shown the ability to pivot when needed to keep our patients safe and our community healthy,” said Roose, chief medical officer at Mercy Medical Center. “That meant responding with changes in protocols and policies when appropriate, and being flexible and innovative with how we deliver care. As we think about this fall, it’s just a continued state of preparedness.”
And there’s reason for caution, he said, as the Delta variant, currently the dominant strain of coronavirus by far, has resulted in increased infections and positivity rates both statewide and locally.
“We’re watching the numbers the Department of Public Health is putting out and keeping our ear to the ground with current trends,” said Colleen Desai, vice president of Patient Care Services and chief Nursing officer at Holyoke Medical Center. “We’re certainly in tune with what’s happening across the nation and, more importantly, what’s happening across our state.
“Significantly, the Delta variant is more infectious and can lead to more severe infections among those unvaccinated. Those numbers are really bearing themselves out when you look at trends across the country.”
“But we’ve done this before,” she was quick to add. “We do expect a little bit of uptick — and, based on what we see, we’re prepared to reopen our command center if need be. We know how to do that if we have to — though we’re hoping we don’t. We’re on standby, keeping our ear to the ground, watching, sort of wait and see.”
Roose noted that the summer’s Delta surge has caused the numbers of COVID hospital patients to increase, although more modestly in Massachusetts than in other states, “and that’s clearly and significantly related to different vaccination rates among different populations.”
Indeed, while the Delta variant is responsible for 83% of new COVID-19 cases nationwide, 97% of those hospitalized with COVID-19 are unvaccinated, according to the U.S. Centers for Disease Control and Prevention.
Since January, the Mass. Department of Public Health has recorded more than 12,600 COVID-19 infections and 496 hospitalizations among those fully vaccinated in the state to date, and a total of 124 deaths — roughly 1 in every 35,000 people who have been vaccinated.
Investigators who developed the COVID-19 Simulator (www.covid19sim.org) — which models the trajectory of COVID in the U.S. at the state and national levels — have applied the tool to analyze potential scenarios in which the Delta variant becomes dominant in every state. Their recently published analysis suggests that the combination of Delta’s high transmissibility, low vaccination coverage in several regions, and more relaxed attitudes toward social distancing will likely lead to a surge in COVID-related deaths in at least 40 states.
“Significantly, the Delta variant is more infectious and can lead to more severe infections among those unvaccinated,” Roose said. “Those numbers are really bearing themselves out when you look at trends across the country. Here in Massachusetts, with relatively higher vaccination rates, we’re somewhat protected from those dramatic increases. That’s a testament to the community accepting vaccination — not just the importance of it, but the safety and efficacy of the vaccines.”
Dose of Reality
Nationally, the outlook is concerning. The simulator suggests an additional 157,000 COVID-related deaths could occur across the U.S. between Aug. 1 and Dec. 31, on top of almost 600,000 recorded through July.
The model projects approximately 20,700 COVID-related deaths in Texas, 16,000 in California, 12,400 in Florida, 12,000 in North Carolina, and 9,300 in Georgia during this period. In contrast, the projected number of COVID-related deaths would remain below 200 in Connecticut, Massachusetts, New Jersey, Rhode Island, and Vermont, the top five states in vaccination rate.

“What we’re seeing is that people who are vaccinated may contract COVID, but it’s less severe, with fewer deaths and hospitalizations.”
“These projections should serve as a warning sign, especially in states that could have higher daily COVID-19 deaths than their previous peaks,” Jagpreet Chhatwal, associate director of Massachusetts General Hospital’s Institute for Technology Assessment and an assistant professor at Harvard Medical School, wrote as lead author of the simulation analysis. “We also hope that our projections can help policymakers bring back mask mandates and further advocate for COVID-19 vaccines.”
Co-author Jade Yingying Xiao, a PhD student at Georgia Tech, noted that, if recent estimates of the reproduction number of the Delta variant are correct, the team’s model implies current levels of social distancing are reducing transmission by 30% to 40%. However, she added, “we can easily foresee this number dropping as we move ahead into the fall months with schools and colleges reopening.”
It’s inarguable, Roose said, that vaccination rates within communities closely parallel COVID’s human impact.
“Now, at least seven states are seeing surges of hospital cases surpassing any of the prior surges at any point during the pandemic. That’s telling — considering this pandemic has infected millions and millions of people — that so many unvaccinated people are being hospitalized so many months later.”
Take Mississippi, for example, where COVID is raging well above any 2020 level. According to tracking from the New York Times, Mississippi ranked second among states for both most cases and most deaths per 100,000 over one week in mid-August, and third in hospitalizations. The state also ranks next to last among both the percentage of the adult population who have received at least one dose of the vaccine and the percentage who are fully vaccinated.
So, Massachusetts’ much higher vaccination level — 74.1% with at least one dose and 64.9% fully vaccinated (both ranking second nationwide) — lends its residents a measure of protection that Mississippi (44.1% and 36.2%) doesn’t have. Even so, Roose said, it’s no time to get complacent. That’s especially true in Hampden County, whose vaccination rate of 51% lags behind the statewide figure of almost 65%.
“Our efforts will continue to encourage all eligible individuals to be vaccinated,” he told HCN. “There remains a significant, albeit shrinking, number of people who have not yet accepted the vaccine, and closing that gap will help our communities, particularly as more variants or more infectious variants may circulate through the rest of the summer and fall months.”
Vaccine boosters may be an important part of the state’s strategy to keep infections down as well, he said.
While some may be surprised by the number of ‘breakthrough’ infections among those vaccinated, in reality, fewer than one-third of 1% of all vaccinated individuals nationwide have been infected, and cases are almost always much milder than equivalent infections in unvaccinated people, who, again, make up about 97% of COVID-19 patients in hospital beds.
“We would strongly encourage people to get vaccinated,” Desai said. “What we’re seeing is that people who are vaccinated may contract COVID, but it’s less severe, with fewer deaths and hospitalizations. So, yes, yes, yes — we’re encouraging people to get vaccinated.”
Staying Vigilant
With that encouragement comes an acknowledgement of the medical community’s role in stemming the COVID tide in Western Mass.
“It’s fair to say we’ve never worked harder in our lives,” Desai said. “It’s been a herculean effort to stay current and stay safe, and we’ve done it with tremendous success. The staff here have demonstrated tenacity and dedication to the community. We have been here for the community and will continue to be here for everyone. It’s been nothing short of amazing, the work that has been done within these walls.”
And it’s not over, which is why the hospital continues to promote mask wearing, hand washing, and social distancing when possible, following public-health guidelines.
“We’re well that aware people have to live,” she added. “I think it’s about balance and caution and knowing who you’re with.”
Roose has begun encouraging people to gird against COVID on a daily basis in the same way they’d check the weather before getting dressed. In other words, “think about who you’ll be around, whether it’s indoors or outdoors, will they likely be vaccinated, and what are the rates of transmission in the community that day or week?”
He said mask wearing, hand washing, and distancing are safety measures as thoroughly proven as wearing a seatbelt in the car — and no less relevant than they were when the pandemic emerged in the public consciousness a year and a half ago.
Dr. Benjamin Linas, a professor of Medicine at Boston University School of Medicine and senior author of the recent simulation analysis, agreed.
“If you are not vaccinated, you are at high risk because of the Delta variant. August 2021 is potentially more dangerous to you than August 2020,” he noted. “If you are vaccinated, you are much safer, but you should still care about this ongoing transmission because it creates the circumstances that generate new variants. If we want to end this pandemic, then all Americans need to be vaccinated — and, at least right now, we should be masking when in public indoor spaces.”




