No Time to Lose Dramatic Improvements in Stroke Response Are Saving, Extending Lives
John Hunt sees plenty of people come through HealthSouth Rehabilitation Hospital with speech and swallowing problems, balance issues, weakness, and a host of other struggles following a stroke.
And he’s always thankful for that.
“The fact of the matter is, 20 to 25 years ago, a lot of people who had strokes died from them,” he told HCN. “We’re seeing a lot more people in rehab now that we wouldn’t have seen back then, because they wouldn’t have been alive.”
That’s because stroke treatment, particularly in the hours — and, hopefully, minutes — directly after the event, has evolved so much in the past 15 years that stroke care has become one of the great success stories in healthcare in the 21st century.
“A lot more patients are getting to the emergency room faster and, if they meet the criteria, getting clot-busting drugs quickly, so that their symptoms resolve, or they’re not as severe as they might have been,” said Hunt, HealthSouth’s CEO.
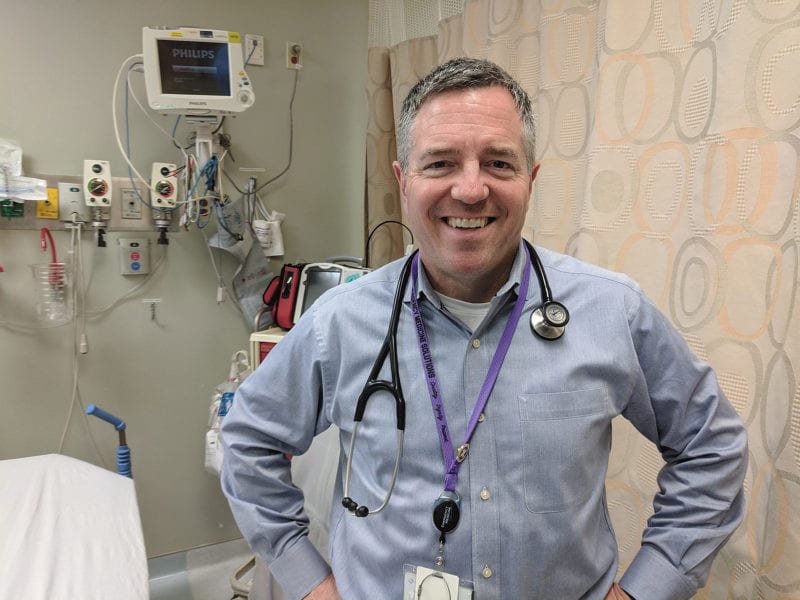
Dr. Louis Durkin knows that story well, because he’s seen the evolution first-hand. Around the time he started working in the ER in 2004, hospitals were just beginning to use thrombolytics, or clot-busting medications, to treat stroke victims.
“When I first started training in the ’90s, there was not a lot you could do for patients who actually had a stroke,” said Durkin, medical director of the Emergency Department at Mercy Medical Center. “It was all about the rehab, physical therapy, and recovering from the stroke, but there wasn’t much to do for the actual incident; it was more about prevention, and then long-term recovery.
“But then, over the past 10 to 15 years, some pretty important modalities for treatment came up,” he went on. “The first one was thrombolytics, medications that break up a clot that causes a stroke.”
Most strokes — about 85{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5}, in fact — are caused by a blood clot that forms in a blood vessel to the brain, what’s known as an ischemic stroke, Durkin noted. (The rest, typically more serious, are hemorrhagic strokes, caused by bleeding into the brain.)
For the former, he said, “if you can break up the blood clot, you can restore blood flow to the brain and therefore save some brain tissue that otherwise would have died. So you can decrease the severity of a stroke if you get to them in time.”
The development of clot-busting drugs turned stroke into a time-dependent emergency, he explained, much like a heart-attack patient needs to get to the cath lab as soon as possible, or responders to a trauma victim need to stop the bleeding.
“In most people, your therapeutic window from the time the stroke starts is about four hours,” Durkin said. “We like to treat them within three hours — sometimes up to four and a half hours, depending on the patient — with thromolytic medications. Stroke has gone from something that was more supportive care to a time-dependent emergency.”
A small subset of ischemic-stroke patients, about 5{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5}, are candidates for a procedure called endovascular clot retrieval, which emerged only in the past decade. If the clot is large enough, the patient may be sent to an endovascular lab — Baystate Medical Center has one, and so does St. Francis Hospital and Medical Center in Hartford — to have the clot physically removed. That, too, is time-sensitive, although the upper limit post-stroke is closer to six hours.
“We still give them thrombolytics, but shift them to removal. That’s been a pretty neat evolution,” Durkin said.
Ticking Clock
Understanding the new focus on time, hospitals have honed their own processes to respond more quickly when someone arrives with a stroke — and they hope they arrive on an ambulance.
“Our pre-hospital coordination is excellent in terms of recognizing stroke,” said Dr. Rajiv Padmanabhan, a neurologist with Baystate Health. “First, we want people to call 911; that’s the main step. Calling an ambulance and EMS makes a big difference in how we treat them.”
Not only can emergency responders work to stabilize a stroke victim on the way to the hospital, he explained, but they can call ahead to make sure the right personnel, scan orders, and medications are in place.
“The concept of ‘time lost is brain lost’ is important for clot-busting medicine, and also for someone who needs clot-retrieval therapy. Both of these are time-sensitive,” he told HCN. “It’s very important for people to recognize and understand that, if you call 911, it improves the communication to enhance the efficiency of the stroke treatments.”
Durkin agreed. “On the first recognition you have a stroke, don’t wait — call 911. Then, when you get to the hospital, we can diagnose the stroke, screen the patient to see if they’re a candidate for the thrombolytic therapy, and get the medication in as soon as possible.”
That begins, however, with recognizing a stroke, so the American Stroke Assoc. continues to educate the public about the acronym FAST, which outlines the signs to look for in someone having a stroke: F, face drooping; A, arm weakness; and S, speech difficulty. If any of those are present, then T kicks in — time to call 911.
“Strokes, for the most part, don’t hurt very much,” Durkin said. “It’s more just a loss of function, sometimes loss of sensation. It’s not very painful, so sometimes patients will ride it out to see if it gets better.”
That’s dangerous, he said, even when the episode isn’t a stroke. Sometimes it’s a transient ischemic attack, or TIA, which lasts a few minutes and causes no permanent damage — but could be a sign that a full-blown stroke is on the way. “It gives you a false sense of security because the exact same thing can happen in a week, and this time it’s a stroke.”
Mercy has significantly honed elements of its stroke response, including posting the fastest average door-to-CT-scan time among large hospitals in Massachusetts. “Most goals at other hospitals is 90{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5} of CT scans done in under 25 minutes. If we’re over five minutes, we start to wonder what’s wrong,” he said, adding that some patients don’t even leave the ambulance stretcher for the scan. Meanwhile, a nurse is already mixing the thrombolytics.
Every step is important, Durkin said. “Every minute lost is hundreds of thousands of brain cells.”
That’s why the American Heart Assoc. and American Stroke Assoc. launched the Get with the Guidelines program, which recognizes hospitals with fast, efficient stroke response. In the Pioneer Valley alone, Mercy, Holyoke Medical Center, Cooley Dickinson Hospital, and Baystate Health’s hospitals are all mainstays on the list of hospitals so recognized each year.
Ahead in the Game
It’s not just about recognition, of course, Hunt said. It’s about saving lives — and improving the quality of lives as well.
“The brain is a pretty amazing thing; it has an amazing ability to heal itself,” he said, adding that stroke patients are not only treated more quickly in the ER these days, they’re often started on a rehab regimen much earlier than years ago.
“We’re now seeing patients in rehab three or four days post-stroke,” he noted. “In the old days, it was 10, 11, even 15 days post-stroke. So much of the old way of thinking, of how aggressive we can be with a patient early on, has changed a great deal in the past 20 years. It used to be, ‘let the patients relax a while, let the brain heal.’ Now we’re getting really aggressive with treatment, using PT, OT, speech therapy, and nursing to address issues early on. And people are going on to productive lives much faster than they used to.”
Because stroke is the number-one cause of disability in the U.S., Padmanabhan said, reducing the impact of stroke basically reduces disability on a large scale.
“We’re making an impact not only immediately, but also three months and six months down the road,” he said — and well beyond that.
That’s good, because the stroke rate, unfortunately, isn’t improving, Hunt said. “We still have more than 800,000 strokes a year in the United States, and that number is not going down. The number of people living and needing help after strokes is going up.”
The silver lining, of course, is that they’re alive. That’s gratifying for Padmanabhan, but even better is not suffering a stroke at all. While they’ll never disappear, individuals can reduce the risk with lifestyle improvements.
“Walk every day. Quit smoking, if you smoke. And talk to your primary-care doctor, at least once a year,” he said. “And remember, stroke can happen at any age, zero to over 100. So if someone shows symptoms of stroke, call 911.”
And let the professionals do their thing — because they’re doing it faster, and more effectively, than ever before.


Comments are closed.