Rehabilitation Is a Key Aspect of Stroke Recovery
There’s no doubt, Sheryl Moriarty says, that hospital emergency departments have become more adept at treating stroke.
“Some great things can happen early on — if the person having the stroke gets to the hospital in time and is treated with tPA clot-busting medications,” she noted.
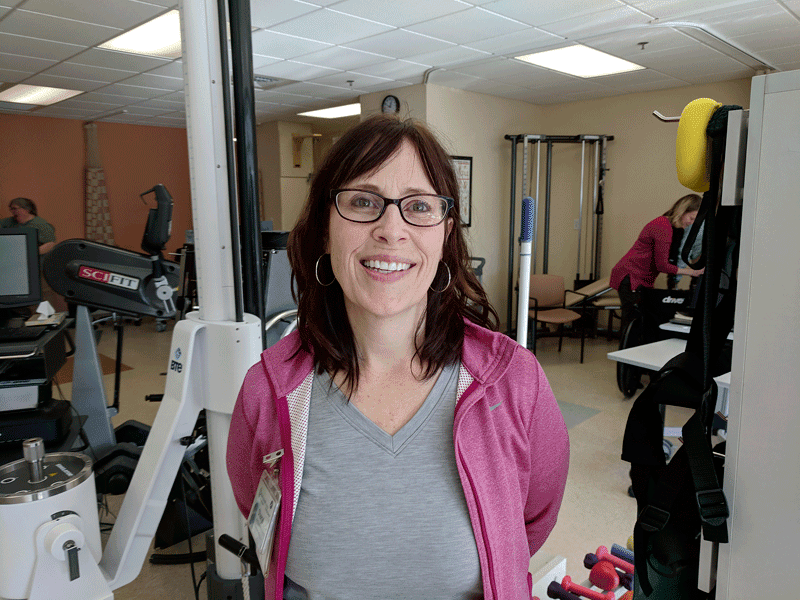
But what if they don’t get help quickly enough, or the stroke is so severe that impairment of brain function is inevitable? In truth, most stroke victims will require therapy — often lots of it, over a long period of time. That’s where people like Moriarty, lead occupational therapist with Weldon Rehabilitation Hospital at Mercy Medical Center, come in.
A stroke is essentially an attack on the brain, caused by interrupted blood flow. There are two kinds of strokes. An ischemic stroke occurs when the blood supply to the brain is blocked by blood clots or plaque build-up; a hemorrhagic stroke happens when a blood vessel in the brain bursts. About 85{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5} of strokes are ischemic. In both cases, brain cells begin to die, and permanent damage may result.
“Recovery from a stroke is not easy,” Moriarty said. “It’s difficult work, and it requires a lot of consistency — almost 24/7 consistency. People can gain recovery up to one or two years — it’s kind of a long road. It depends on where in the brain the stroke happened; that designates what’s going to be impaired.
“Sometimes it’s more visual, or spatial awareness,” she went on. “You can have incontinence, bowel- and bladder-related issues related to muscle spasms, swallowing issues, issues with the upper extremities, lower extremities, motor issues — it does vary. But you get the majority of recovery and the best window of opportunity generally in the two weeks to six months after a stroke; that tends to be a big, big piece.”
Courtney Brown, a physical therapist with Baystate Rehabilitation Care, also works with outpatient stroke survivors who have been in the hospital already, and who may have already gone through inpatient rehab, either at a skilled-nursing facility or a specialty rehab center like HealthSouth.
“Sometimes they’ll go home from there and receive home therapy, but come here for rehab services,” she noted, adding that she sees stroke-recovery patients of all levels of need. “They can be ambulatory or in a wheelchair. We see mostly older people, in their 80s and 90s, but we’ve seen strokes in children. We’ve actually had more people recently in their late 40s, 50s, and 60s.”
Brown’s department, which focuses on neurological patients recovering from strokes, traumatic brain injury, Parkinson’s, and other conditions, offers a range of physical, occupational, and speech therapies, she noted before describing each category.
For physical therapy, she explained, the focus is on gait, mobility in and out of bed, balance, and bracing, for starters. “If someone has a drop foot from their stroke, we work on orthotics, we help with gait and transfer, we do strengthening and stretching.”
Occupational therapy works more on the upper body, she explained, and this is where patients relearn how to manage the activities of daily life. Speech therapy targets any number of issues, from swallowing to cognition, problem solving, and memory. “If people are aphasic, we help with the speaking piece of that or the cognitive piece of processing language.”
The providers who work with stroke patients have to be adept in many different modalities, because no two stroke patients are the same. But in a medical world that has become increasingly high-tech, therapists still rely very much on basic, time-tested methods — and a lot of hard work from the survivors themselves.
Back to Basics
There are a few high-tech tools at therapists’ disposal, Moriarty noted, from electronic stimulation to retrain muscles to MRIs, which help target affected areas of the brain. “Other parts of the brain can pick up the role of a damaged part, but it takes a lot of repetition, a lot of consistency, and a lot of work.”
Other tools are decidedly low-tech, from constraint therapy — putting a mitt on one hand so the patient relearns how to use the side of the body most impaired by the stroke — to mental imagery, in which the therapist or an audio recording trains the survivor to visualize himself or herself carrying out a function, like picking up a glass, before actually doing it.
“There’s really not a cost to that; it’s that simple,” she added. “You don’t necessarily need all the high-tech stuff. A lot of places don’t have it.”
Brown said Baystate focuses on the basics as well. “Some people have more high-tech things, but we tend to focus on trying to gain that strength and function back. We break it down to the functional level, to determine what the patient wants. Whether their goals are to get into bed, use the toilet, be able to walk around the house, or get dressed on their own, we use a functionally based approach.”
And it’s definitely not easy.
“The majority are 65 to 85, not that we don’t see them younger,” Moriarty said. “These are people who retired, they’re not getting up for work every day, maybe they’re not used to doing exercise, and it’s hard work — ‘I almost died, and now I have to do six hours of therapy.’ There’s a little dismay there.”
For that reason, there’s a certain emotional-support and motivational aspect to an outpatient therapist’s job, and also an educational element, since they can’t be there all the time.
“We definitely give people exercises they can continue to work on at home,” Brown said. “They come in twice a week, which is not quite enough to fully gain back that function, so we give them exercises to help them with that.”
In addition, she said, “we often have family members come in for sessions, and give them education, too, on how to continue practicing these things. We also give them basic education on how stroke can affect somebody and how every recovery is different. You can’t expect two people with stroke to have the same timeline for recovery and have the same function.”
Support groups help as well, she added. “It can be nice to see different people all going through something similar. They see they’re not alone.”
By the Numbers
You’ve probably heard the numbers. Stroke, the number-five cause of death in the U.S., kills nearly 130,000 people each year — one in every 20 deaths — while roughly 795,000) people in the U.S. have a stroke every year, with about three in four being first-time strokes.
To break that down, someone in this country has a stroke every 40 seconds, and someone dies of stroke every four minutes.
The risk varies by demographic. Three-quarters of all strokes strike people over 65. About 60{06cf2b9696b159f874511d23dbc893eb1ac83014175ed30550cfff22781411e5} of deaths from strokes occur in females, while African-Americans are more impacted by stroke than any other racial group within the American population.
The risk can be reduced, of course, through certain lifestyle adjustments. Risk factors for stroke range from high blood pressure, smoking, and a high level of bad (LDL) cholesterol to diabetes, heart disease, overweight and obesity, poor diet, physical inactivity, and excessive use of alcohol. Atrial fibrillation (irregular heartbeat) is also a risk. In young people, illicit drugs like cocaine are a common cause of stroke. Sickle-cell disease, family history of stroke, and migraine headaches may also raise the risk.
But when a stroke does strike, the therapy offered by the teams at Weldon, Baystate, and myriad other sites around the region are key to helping survivors get their function back. Brown finds the process gratifying.
“Someone might have been in the hospital for a week, then rehab for two weeks, and we get to see them further out, but they still have a lot to gain,” she said. “We’ll see people come in initially using a wheelchair or assistive device like a walker or cane, and leave not needing that anymore. It’s nice when they can get back to their daily lives.”


